Best Medical Billing Companies in Georgia

In Georgia, it is important to choose the right medical billing partner to make sure your practice grows and follows the rules. Your ideal partner should increase your revenue from claims, reduce the number of denied claims, and simplify administrative tasks. Medical billing is a big problem for healthcare practices in Georgia. There are some complications in provider credentialing in Georgia, including complicated […]
Best Medical Credentialing Companies in USA 2025

Credentialing providers is foundational for quality patient care, efficient revenue cycle management, and adherence to payer standards. Whether you’re a solo practitioner, a group practice, or part of a facility network, partnering with the right credentialing firm can streamline onboarding, accelerate payment turnaround, and minimize payer enrollment errors. In 2025, more providers are outsourcing credentialing […]
Best Medical Credentialing Companies in Maryland

Why Credentialing is Crucial for Maryland Providers The process of verifying the credentials of healthcare providers is known as credentialing. In Maryland, there are strict regulations that providers must follow. They need to possess the appropriate licenses and educational qualifications, and they must meet the requirements set by payers. Any failure to comply with these […]
What is Modifier GZ in Medical Billing?
Medical billing is a complex and tricky field, and with Medicare, accuracy and compliance are crucial. Modifier GZ is one such compliance tool, as it is a code that explicitly tells the Medicare administration that a claim should be denied. Why, then, would any provider submit a claim they know will be denied? The answer […]
What is Modifier XU in Medical Billing?
Transparency and conformity are all that matter in medical billing. Modifier XU is used when the coder needs to provide an accurate description of the unique procedural services that otherwise would be coded under the standard coding edits. As the subdivision of X modifiers introduced by the Centers for Medicare & Medicaid Services (CMS), Modifier […]
What is Modifier XP in Medical Billing?

In medical billing, Modifier XP has proven to be very important for accurate claims processing. Especially when many providers treat patients in the same group on the same day. Coding is becoming more complicated, and enforcement by payers is increasing. It’s necessary to learn how to use this modifier correctly. The Centers for Medicare & Medicaid […]
Acupuncture CPT Codes 2025: Billing Guidelines & Tips
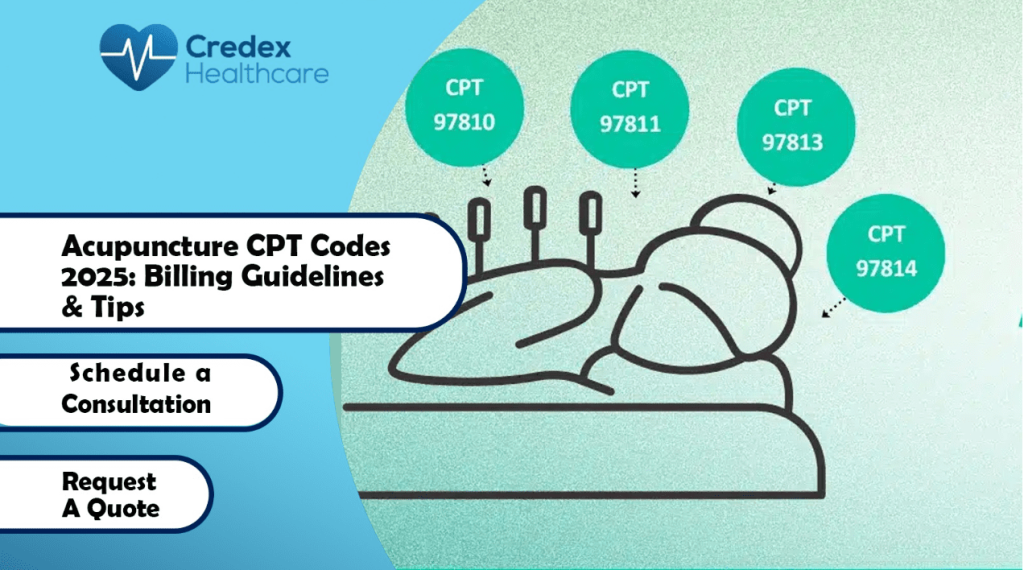
What Are CPT Codes for Acupuncture? CPT codes for acupuncture are a set of numbers that tell payers what service was given. Acupuncturists use these codes to bill insurance. The main codes are 97810 and 97811 for manual acupuncture. They also use 97813 and 97814 for electroacupuncture. Each code covers a session of needling. The […]
Understanding Contractual Adjustments in Medical Billing: A 2025 Guide
What Is a Contractual Adjustment in Medical Billing? A contractual adjustment in medical billing refers to the portion of a medical bill that a healthcare provider agrees not to collect. This happens because of a contract between the provider and the insurance payer. Credex Healthcare helps Maryland providers and billing teams manage these adjustments. When […]
Best medical billing companies in Michigan in 2025

Introduction Identifying a reliable medical billing partner in Michigan can be challenging. You need a team that understands your practice’s unique billing needs—from claims submission to coding accuracy. Complex payer requirements and uninsured patient populations may complicate payment collections. Partnering with a top-tier billing service provider can help resolve these challenges efficiently. Credex Healthcare – […]
Best medical billing companies in California

Introduction Success as a medical provider in California hinges on balancing patient growth with financial sustainability. With continually evolving coding standards, payer policy variability, and state-specific regulations, managing revenue cycle functions internally can quickly strain internal resources. Outsourcing billing to a reputable partner can reduce operational costs, improve cash flow, lower claim denials, and allow […]




